Vestibulum luctus odio
May 28, 2020
Synthetic Bone Grafts
July 19, 2021Comparative Evaluation of β-TCP Putty and Platelet Rich Fibrin in Treating Furcation Defects
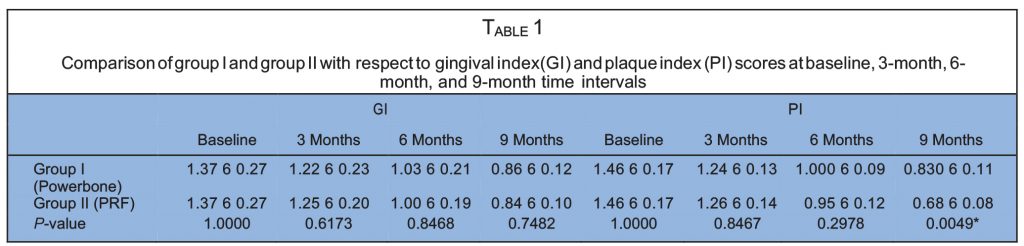
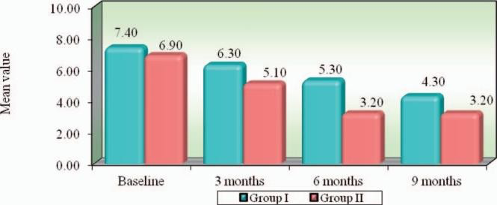
The aim of this study was to compare a second-generation β-TCP putty biomaterial against platelet rich fibrin in treating grade II furcation defects. Subjects were 15 systemically healthy patients (10 males and 5 females, ages 20–50 with a mean age of 38.33) with 20 mandibular molar class II furcation defects according to Glickman’s classification. The 20 mandibular molar furcation defects were randomly allocated as follows: Group I, 10 furcation defects weretreated using β-TCP (Powerbone) bone graft putty material; Group II, 10 furcation defects were treated using platelet rich fibrin (PRF). Customized acrylicstents were fabricated on study casts and trimmed to the height contour of the teeth to serve as a fixed reference point for measurements. The followingmeasurements were collected: gingival index, plaque index, vertical probing depth (from gingival margin tobase of the pocket), clinical attachment level (CEJ tothe base of the pocket), and horizontal probing depth of furcation involvement (using stent). Results showed that both groups had improvement in gingival index (GI) and plaque index (PI) at the recall intervals. There was an overall reduction in both vertical and horizontal probing depth in both groups;however, the Putty group (Group I) showed consistently more vertical probing depth reduction than the PRF group (Group II) at the end of third month (P-value¼ 0.0004), sixth month (P-value¼ 0.00001), and ninth month (P-value¼ 0.0004). Our conclusion was that use of β-TCP osteostimulative biomaterial yields superior clinical results, including increased pocket depth reduction of class II furcation defects as compared to an autologous platelet concentrate. Theclinical significance of our findings includes the ease of use and superior biologic performance of second-generation putty β-TCP biomaterials in furcationdefects.
INTRODUCTION
periodontal Regenerative aims to regenerate the attach- ment apparatus: bone, cementum, and periodontal ligament. Clinical outcomes defining successful regen- erativetherapyinclude reductioninprobingdepth, gain
in clinical attachment level, and radiographic evidence of bone fill.1 Management of furcation presents one of the major challenges in periodontal treatment. Teeth with furcation involvement undergo more extensive, rapid clinical attachment loss and are lost with greater frequency thansingle-rooted teeth.2 A wide range of graft materials have been applied and evaluated clinically, including allografts, xenografts, and syn- thetic/semi-synthetic materials.2 Platelet rich fibrin (PRF) is an autologous biomaterial containing leukocytes, platelets, and a wide range of keyhealing proteins within a dense fibrin matrix. PRF holds promise as a regenerative material as it releases high amounts of growth factors (TGFb1,PDGF-AB, VEGF) and matrix glycoproteins. Thus it may enhance proliferation of different
MATERIALS AND METHODS
The present study was conducted in the Department of Periodontology, Rajarajeswari Dental College and Hospital, Bangalore, India, and the study design was approved by the Ethical Committee of Rajarajeswari Dental College and Hospital. Fifteen systemically healthy patients were selected for the study (10 males, 5females, ages 20–50 years with a mean age of 38.33) with 20 mandibular molar class II furcation defects, according to Glickman’s classification.
The inclusion criteria for the study was presence of Glickman’s grade II furcation defects in mandibular molars, with a radiolucency in thefurcation area, a probing depth (PD) ≤5 mm and horizontal PD ≤3 mm. The patients were in good systemic health and had not undergone any periodontal surgery in the areas to betreated within the prior 12 months. The participants had with no known allergy to materials/drugs used or prescribed in this study.
Weexcluded patients who were smokers, used alcohol, on any medications taken within the prior 6 months that could alter the periodontalstatus, and pregnant or lactating mothers.
The 20 mandibular molar furcation defects that were selected were randomly allotted to one of the 2 groups:
- Group I: 10 furcation defects were treated using β-TCP (Powerbone) bone graft putty
- Group II: 10 furcation defects were treated usingplatelet rich fibrin (PRF).
Informed consent was procured from each patient, and each was scheduled for surgery following an initial phase of therapy, including oral hygiene instructions and scaling/root planing. Occlusal adjustments were performed whenever necessary.
cell types, including fibroblasts, osteoblasts, adipocytes, and keratinocytes.3
Alloplastic biomaterials are biocompatible inorganic syn- thetic bone grafting materials; types include nonporous and porous hydroxyapatite,beta tricalcium phosphate, polymethyl- methacrylate, hydroxyethylmethacrylatepolymers, and bioac- tive glasses. The outcome ofalloplasticbonegrafting materials is dependent primarily on their chemical composition, structure, and physical properties.4,5 Recently, putty formulations of β-TCP with glycerin and polyethylene glycol as an additive have received significant attention due to the combination of their osteostimulative and osteoconductive properties with superior handling characteristics and ease of use in grafting osseous defects.5,6 This putty form of β-TCP enhances the handling characteristics of the graft.5–7 It is a premixed composite of bioactive calcium phosphosilicate particulate and a synthetic, absorbable binder. The bioactive particulate is composed solely of elements that exist naturally in native bone (Ca, P, Na, Si, O).7
Clinical measurements
Customized acrylic stents were fabricated on study casts and trimmed to the height of contour of the teeth, to serve as a fixed reference pointto take measurements. All measurements in this study were performed using a UNC-15 periodontal probe and a graduated Naber’s probe. All measurements were rounded off to the nearest millimeter, and clinical measure- ments were performed by a single examiner to avoid interexaminer variation. The following clinical parameters were recorded at baseline, 3, 6, and 9 months postsurgery:
- Gingival index (Loe & Silness, 1963).
- Plaque index (Silness & Loe, 1964). Soft tissue parameters:
- Vertical probing depth (from gingival margin to base of the pocket).
- Clinical attachment level (CEJ to the base of the pocket).
- Gingival margin position (using stent).
Hard tissue parameters: horizontal probing depth of furcation involvement (using stent).

Surgical protocol
The patient rinsed with 0.2% chlorhexidine digluconate mouth rinse for 30 seconds prior to surgery. Local anesthesia was obtained using 2%xylocaine. Sulcular incisions were made on the buccal and lingual. A full thickness mucoperiosteal flap was raised to provide access to the defect and the surrounding alveolar bone. Debridement of granulation tissue from the osseous defect and furcation with ultrasonic, hand scaling, and root planing of all the exposed root surfaces was performed. Furcation defects were thoroughly scaled/root planed with hand instruments andultrasonic scalers. Following removal of granulation tissue, the surgical area was irrigated with normal saline and carefully inspected for any remaining granulation tissue or deposits; re instrumentation was performed if required. The defects were filled with PRF at the control sites.
At the experimental site, the defects were filled with bone graft material. The required quantity of bioactive graft material was transferred from syringe and delivered into the defects. In both cases, small increments of graft material were added and properly condensed until the defect was completely filled. Flaps were repositioned and secured in place using 3-0 nonabsorb- able silk inan interrupted pattern. Surgical siteswere protected with a non–eugenol periodontal dressing (Coe–Pak, GC America, Alsip, Ill). All patients were prescribed systemic Amoxicillin 500 mg for 3 days, thrice daily, along with ibuprofen tablets. Postoperative instructions were given, and patients were instructed to report back 24hours after surgery and again after 10 days.
At 10 days postsurgery the sutures were removed. The patients were evaluated clinically and radiographically at 3-, 6-, and 9-month intervals.The customized acrylic stent was placed on each defect site. Using UNC–15 graduated periodontal probe and Naber’s probe, measurements ofattachment gain, pocket depth, and furcation depth were retaken, similar to the presurgical measurements.
DISCUSSION
In the present study, 20 grade II mandibular furcation defect patients were included and randomly allotted into 2 groups of 10 defects each, treated with either PRF (Group I) or β-TCP Powerbone Putty (Group II) as a graft material. The PI and GI scores showed a statistically significant reduction in both groups at 9 months postoperatively.
Statistical analysis
Clinical parameters were recorded at baseline and at 9 months postsurgery, and suitable statistical analyses were performed to compare the parameters. Intergroup comparisons of all the clinical parameters between Group I and Group II (except for bonedensity changes) were madeusing Mann-Whitney U test, and the intragroup comparison of clinical parameters was performed using the Wilcoxon matched pair test. The intergroup comparison of the bone density changes was analyzed using Student’s t-test.
RESULTS
Both treatments showed improvement in gingival index (GI) andplaque index (PI) at the recall intervals, and the PI scores at the 9-month interval of Group II (Powerbone) showed better reduction than that of Group I (PRF). There was an overall reduction in both vertical and horizontal probingdepth in both groups; however, vertical probing depth reduction in Group II showed better statistically significant results than did Group Iat theendof 3 months (P¼0.0004), 6 months(P¼0.00001), and 9 months (P ¼ 0.0004). Reduction in horizontal probing depth intergroup showed no statistically significant difference. However, the intergroup showed statistically significant im- provement in the gingival margin position andimprovement in clinical attachment in Group II when compared to Group I. Radiographically, the β-TCP putty group showed better improvement in bone fill over the sites treated with PRF with statistically significant differences at 6- and 9-month intervals (Tables 1 through 3, Figures 1 through 4).
Clinical measurements
Customized acrylic stents were fabricated on study casts and trimmed to the height of contour of the teeth, to serve as a fixed reference pointto take measurements. All measurements in this study were performed using a UNC-15 periodontal probe and a graduated Naber’s probe. All measurements were rounded off to the nearest millimeter, and clinical measure- ments were performed by a single examiner to avoid interexaminer variation. The following clinical parameters were recorded at baseline, 3, 6, and 9 months postsurgery:
- Gingival index (Loe & Silness, 1963).
- Plaque index (Silness & Loe, 1964). Soft tissue parameters:
- Vertical probing depth (from gingival margin to base of the pocket).
- Clinical attachment level (CEJ to the base of the pocket).
- Gingival margin position (using stent).
Hard tissue parameters: horizontal probing depth of furcation involvement (using stent).
MATERIALS AND METHODS
The present study was conducted in the Department of Periodontology, Rajarajeswari Dental College and Hospital, Bangalore, India, and the study design was approved by the Ethical Committee of Rajarajeswari Dental College and Hospital. Fifteen systemically healthy patients were selected for the study (10 males, 5females, ages 20–50 years with a mean age of 38.33) with 20 mandibular molar class II furcation defects, according to Glickman’s classification.
The inclusion criteria for the study was presence of Glickman’s grade II furcation defects in mandibular molars, with a radiolucency in thefurcation area, a probing depth (PD) ≤5 mm and horizontal PD ≤3 mm. The patients were in good systemic health and had not undergone any periodontal surgery in the areas to betreated within the prior 12 months. The participants had with no known allergy to materials/drugs used or prescribed in this study.
Weexcluded patients who were smokers, used alcohol, on any medications taken within the prior 6 months that could alter the periodontalstatus, and pregnant or lactating mothers.
The 20 mandibular molar furcation defects that were selected were randomly allotted to one of the 2 groups:
- Group I: 10 furcation defects were treated using β-TCP (Powerbone) bone graft putty
- Group II: 10 furcation defects were treated usingplatelet rich fibrin (PRF).
Informed consent was procured from each patient, and each was scheduled for surgery following an initial phase of therapy, including oral hygiene instructions and scaling/root planing. Occlusal adjustments were performed whenever necessary.